In order to survive, a parasite must usurp the resources of another organism to grow and reproduce. Many parasites accomplish this task by partially debilitating their host while still keeping it healthy enough to continue providing shelter and nourishment. But one organism in particular has elevated its control over the host to new levels.

Cats are the typical host of T. gondii but many other warm blooded animals can also carry the parasite.
The tiny, unicellular parasite, Toxoplasma gondii, has the ability to remodel its host’s brain and induce behavior that is beneficial to its proliferation. This induced behavior emboldens rodents to approach predators without fear, essentially a suicidal tactic for the animal. The deadly neurological changes that occur under the infection cause mice and rats to willfully walk to their death. And as if that weren’t enough, T. gondii is known to affect humans.
The T. gondii protozoan was first identified in 1908, when two French scientists, Nicolle and Manceaux, discovered it in a North African rodent called the gundi (1). They named Toxoplasma gondii for the form of the parasite during its infectious stage. Toxon is latin for “bow” or “arc,” plasma translates to “life” and gondii refers to its discovery in the gundi (6). In fact, the correct name for the parasite should be Toxoplasma gundii, as Nicolle and Manceaux had incorrectly identified the host as Ctenodactylus gundi instead of Ctenodactylus gondi (1). But the erroneous name stuck, and by 1937 scientists realized that T. gondii was a versatile infective agent that could affect any mammal.
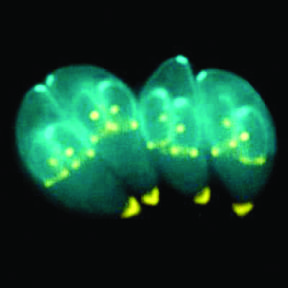
The life cycle of T. gondii consists of several stages. The tachyzoite form invades a host’s cells and replicates quickly to spread the toxoplasmosis infection. It then forms latent tissue cysts in the host containing the bradyzoite. Finally, sexual production results in the sporozoite, which is found in the oocysts and spread through cat feces (2).
The definitive host of T. gondii is the cat, as this is the only organism that sheds oocysts in its feces and thus completes the protozoan’s full life cycle. However, any other mammal can act as a carrier by either consuming feline feces or by eating T. gondii in tissue. The infection is so versatile in host preference that it was not discovered in cats, the definitive host, until 1942 (1). As a result of these transmission vectors, the intermediate rodent hosts that fall prey to cats are evolutionary targets of a T. gondii adaptation that causes neurological changes in order to increase the likelihood that the cat ingests infected mice, thus returning the parasite to its true host (3). Carnivorism of rodents is believed to be the most prevalent mode of transmission back into cats from other species (2).
Healthy rats have a highly developed innate aversion to predator odors, as do even naïve laboratory rats that have never been exposed to predators (3). But in a study in which laboratory rats were infected with T. gondii, the rats stopped avoiding cat urine while remaining otherwise healthy, indicating that a change occured specifically in the brain. In fact, affected rats developed an attraction to the cat odor, with little change in behavior toward rabbit odor (a mammalian non-predator control) (3). Other research has proven that infected rats exhibit a significant attraction to cat urine over mink urine, even though both are predators (4).
After a rodent ingests the parasitic oocysts, thin-walled cysts form in the brain and persist for the life of the host. While the mechanism responsible for the behavioral change is not fully understood, one possibility is that the cysts block anxiety-inducing N-methyl-D-aspartate (NMDA) receptors in the brain. Experiments showed that artificially blocking NMDA receptors results in behavior similar to that of T. gondii rodent hosts (3). Other potential targets are serotonin (5-HT) agonists, which can temper the anxiety response to predators.
Today, an estimated 2 billion people are chronically infected with T. gondii, comprising 30 to 50 percent of the population (2). The infection, called toxoplasmosis, was originally believed to be asymptomatic in humans, but recent studies have linked the parasite to several psychiatric disorders such as Parkinson’s disease and schizophrenia.
The first definitive case of toxoplasmosis in humans occurred in 1938, when an infant girl in New York City began experiencing convulsive seizures three days after birth. She died within a month, and the autopsy revealed T. gondii cells in her brain, spinal cord, and retina (1). Even though the girl’s mother was an asymptomatic carrier of the infection, the girl was killed because congenital toxoplasmosis has the most striking phenotype in humans, affecting the brain during the critical stages of development and causing mental retardation, seizures, and vision loss (2). In fact, since the parasite can transverse the placenta, many pregnancies in women with toxoplasmosis result in stillbirths or abortions. Toxoplasmosis infections early in pregnancy are more likely to cause abortions, while infection in later trimesters can result in a viable but neurologically impaired phenotype for the child (5).
Acquired toxoplasmosis generally has a milder phenotype in humans, but has recently been implicated in serious psychological disorders. Many people with acquired infection are asymptomatic, but others, especially children, exhibit neurological symptoms similar to those of congenital toxoplasmosis. The first reported case of acquired infection occurred in a six-year-old boy in 1941, who was first admitted for headaches and convulsions after being struck in the head with a baseball bat. Doctors discovered that by coincidence he had recently been infected with toxoplasmosis, which led to encephalitis (acute inflammation of the brain) that killed him within a month. (1)
The AIDS epidemic of the 1970s compounded the effects of toxoplasmosis, as a compromised immune system allows latent bradyzoites to convert back into the aggressive tachyzoites, resulting in continuous flare-ups of infection (2,6). Comorbidity of toxoplasmosis with AIDS commonly leads to toxoplasmic encephalitis of the central nervous system.
More recently, T. gondii has been implicated as a contributing factor to chronic psychological disorders. Association studies have shown that schizophrenia, Parkinson’s disease, cryptogenic epilepsy, and migraine are all linked to toxoplasmosis infection (7,8). These diseases have a clear environmental element.
Epidemiological studies of schizophrenia have shown that infection, winter-spring birth, and urban birth are correlated with the condition. Psychiatric symptoms are a known consequence of acquired toxoplasmosis. For example, an affected 22-year-old woman exhibited disorganized speech and “said she had no veins in her arms or legs.” Other patients had visual and auditory hallucinations accompanied by thought disorder. Several studies have shown that T. gondii infection is associated with schizophrenia, and two studies even showed that adults with bipolar disorder or schizophrenia had a greater exposure to cats during childhood (7).
T. gondii selectively damages glial cells of the brain in humans, a cell-type that is thought to be a contributing factor to schizophrenia. Additionally, infection modulates levels of several dopamine and norepinephrine, which are associated with neurological disorders (7). The effect of T. gondii on dopamine may also be the contributing factor to its association with Parkinson’s disease, where loss of dopaminergic neurons leads to the decrease in psychomotor skills (8). While T. gondii may not affect humans in the same deliberate and deadly manner as it does in mice, research indicates that it indeed has the ability to modify human brains as well, sometimes with devastating consequences.
Free will is one of the tenets of life that we hold paramount, and even at times take for granted. But the tiny Toxoplasma gondii has proven itself capable of commandeering an entire animal, and reducing it to a vehicle that will deliver it back into the stomach of a cat. The helplessness of a rodent willfully presenting itself to its executioner is a disturbing feat of nature. Furthermore, this adaptation of T. gondii is a testament to the seemingly boundless potential of evolution. To induce such a specific behavior on an organ as complex as the brain is an exploit that human technology is not yet able to rival. But luckily for us, the dangers of T. gondii in humans are less immediate, though still formidable. For now, it serves as a demonstration of the power in evolutionary adaptation.
References
1. J. P. Dubey, J. Eukaryot. Microbiol. 55, 467-475 (2008).
2. M. Gulinello et al., Microb. and Infect. 20, 1-10 (2010). (Epub ahead of print)
3. M. Berdoy, J. P. Webster, D. W. Macdonald, Proc. R. Soc. Lond. B. 267, 1591-1594 (2000).
4. P. H. L. Lamberton, C. A. Donnelly, J. P. Webster, Parasitology 135, 1143–1150 (2008).
5. J. G. Montoya, O. Leisenfeld, The Lancet 363, 1965-1976 (2004).
6. D. J. P. Ferguson, Mem. Inst. Oswaldo Cruz, Rio de Janeiro 104, 133-148 (2009).
7. E. F. Torrey, R. H. Yolken, Emerging Infect. Dis. 9, 1375-1380 (2003).
8. O. Miman et al., Neuroscience Letters 20, 1-3 (2010). (Epub ahead of print)