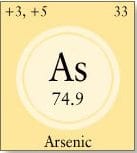
What is Arsenic?
Naturally occurring in the Earth’s crust and widely dispersed in the environment, arsenic is the 20th most abundant element.
In nature arsenic is usually found in sedimentary or igneous rock joined to or mixed with other elements, such as oxygen. Arsenic has a particular affinity for sulfur and is often found joined to sulfur in ores – mixtures of minerals that are mined for profitable materials such as silver or copper. The common ore arsenopyrite, a rusty red rock, is a combination of arsenic with sulfur and iron. This ore, known since the Greeks of Aristotle’s time, is an important commercial source of arsenic.
A less common form of arsenic found in nature is the silver-gray rock called arsenic trioxide, which also goes by several common names including elemental, native, pure and white arsenic. Arsenic trioxide is also important as a raw material for products containing arsenic.
Because arsenic is an element like carbon and oxygen it does not break down in the environment into simpler substances -though it can change form and combine with other elements into molecules that have different chemical properties. Some forms of arsenic are quite toxic; others are less so.
Most arsenic compounds are undetectable to the senses, since they have no smell or taste. But when arsenic is heated – by bright sunlight or in a laboratory experiment – it passes directly from its solid state to a gas and gives off a distinctive garlic odor. Miners once recognized arsenic in rock by the pungent aroma released by blows of a hammer or pick.
Though arsenic is often grouped among the toxic metals, it belongs to a class of elements known as metalloids, which share properties of both metals and nonmetals.
Why Are we Concerned About Arsenic?

Until recently, arsenic was believed to be a concern primarily for workers who produced or used arsenic-containing products. People who came into contact with concentrated sources of arsenic such as industrial or agricultural wastes or arsenic-based pesticides or medicines were also thought to be at risk.
More recently, exposure to arsenic from natural sources in the environment has become a concern. In the early 1990s, an unprecedented arsenic poisoning in Bangladesh brought international attention to the toxic effects of naturally occurring arsenic in drinking water. In an effort to solve the problem of unreliable and unsafe drinking water in Bangladesh, several international agencies had supported a program that replaced shallow surface-water wells with deeper, drilled wells. This reduced epidemics of cholera and other water-borne diseases in Bangladesh, but years later a new pattern of illness emerged in the population. Eventually, these illnesses were traced to the drilled wells, which were tapping water contaminated by arsenic from underground rock. The World Bank and UNICEF are now providing Bangladesh financial support to develop alternative drinking water supplies from sources such as stored rainwater or treated pond water.

In recent years, exposure to arsenic in drinking water has also been identified as a health concern in regions of the United States where bedrock contains unusually high levels of arsenic, such as areas of New Hampshire, Maine, Michigan and regions in the Southwest and Rockies.
Scientific advances including new techniques for accurately measuring small amounts of arsenic in rock and in water are now enabling scientists to detect the presence of arsenic with accuracy and to assess the long-term effects of relatively low levels of arsenic on ecosystems and human health.
Who is at Risk of Harm from Arsenic Poisoning?

In the past, people exposed to arsenic in the workplace were at greatest risk of arsenic poisoning. People involved in the mining, processing or smelting of arsenic ores and people involved in the manufacture or use of arsenic-containing pesticides often inhaled arsenic on the job. Their risk of developing lung cancer was high, and even higher if they also smoked cigarettes. Tobacco itself contained high levels of arsenic until recently, due to the extensive use of arsenic-based pesticides in tobacco farming. Workers who inhaled arsenic on the job often came into contact with arsenic through the skin as well. European vineyard workers until the 1940s used arsenic-based pesticides extensively; many developed skin cancer as well as other illnesses.
Because of concerns about the effects of arsenic-based products on human health and the environment, many uses of arsenic have been curtailed. Industries that still use or process arsenic have initiated safety precautions for workers.
Today the exposure of greatest concern in the U.S. and throughout the world is from arsenic-contaminated drinking water. Of less concern, but still a risk, is exposure to arsenic by sawing, sanding or burning wood treated with arsenic-containing preservatives (CCA-pressure treated lumber).
Where is Arsenic Found?

All of the natural forms of arsenic can be traced back to geological deposits. On average, there are about two parts arsenic for every million parts of rock or soil on Earth (a measurement usually expressed as two parts per million or 2 ppm). But arsenic is not distributed evenly throughout the globe.
Sedimentary rock in some areas, such as regions of India, China and South America, may contain as much arsenic as two parts per hundred – two percent by weight. Higher-than-average concentrations of arsenic have also been found in the underground rock of some areas in the United States, such as areas of New Hampshire, Maine, Michigan and several Western and Southwestern states. Arsenic in these regions sometimes appears in bedrock as concentrated streaks or veins. Under certain conditions, arsenic from geological formations may leach into groundwater.

Nature transports arsenic from place to place through the weathering of arsenic-rich rock and through underground processes that depend on the chemistry and composition of soils and rock. Humans have produced concentrated sources of arsenic by digging it up, using it, and moving it around. Such activities include mining arsenic-containing ores, and smelting – heating those ores – to extract copper, silver or gold. (Arsenic could be collected, in pure form, from the interior of smelter smokestacks.) The arsenic was often left behind in piles called tailings, creating concentrated waste sites. Of course in some cases miners were seeking the arsenic itself. The past use of arsenic-containing pesticides or other agricultural chemicals as well as air emissions and wastes from ammunition, glass and chemical manufacturers have also dispersed arsenic into the environment.
Toxic waste sites including areas designated by the U.S. Environmental Protection Agency as Superfund sites often contain high amounts of arsenic in combination with other toxic wastes. One such site – the focus of the film A Civil Action – is the watershed of the Aberjona River near Boston, Mass., where wastes from tanneries and other factories were discharged for more than a century. Lake sediments in the region have been found to contain as much as one to two percent arsenic by weight.
What are the Uses of Arsenic?

Arsenic has a long history as a poison- a rodent poison in particular – and great lore as a homicidal agent. Humans have exploited its toxic properties in weed killers, fungicides and insecticides, especially in vineyards, apple orchards, and cotton and tobacco fields. Arsenic has also been used as an embalming agent, to preserve specimens in taxidermy and to defoliate cotton for harvesting.
Beginning in the late 1700’s, arsenic was used as a pigment in paintings, fabrics and wallpaper. One popular pigment, called Scheele’s green after the Swedish chemist who invented it, was a bright green hue made from copper arsenite.

In the 18th and 19th centuries, ammunition manufacturers added arsenic to melted lead and dropped the mixture from tall “shot towers.” Arsenic increased the surface tension of the molten lead, producing more rounded shot. Shot towers have become historic sites in many cities, including Baltimore, Philadelphia and San Francisco. After years of use, the areas around these towers often became heavily contaminated with arsenic. Arsenic compounds have been used medicinally at least since the time of Hippocrates in the fifth century. One of the best-known arsenical preparations was a one-percent solution of potassium arsenite called Fowler’s Solution, which was used beginning in the 19th century to treat skin diseases, syphilis, digestive problems and other internal ailments. Unfortunately, it became apparent that people who used Fowler’s had a significantly elevated incidence of cancer; this was most apparent in those who applied it to their skin, who subsequently developed skin cancers at those sites. Its use was phased out between the 1930s and 1950s.
A number of medical formulations containing arsenic were developed in the early twentieth century but most uses were suspended in the 1940’s and 1950’s. One arsenical preparation that is still in use is a drug called melarsaprol, which is prescribed to treat African sleeping sickness. According to the U.S. National Safety Council the major use of arsenic in the United States today is as the wood preservative in CCA (chromated copper arsenite) pressure-treated lumber. Arsenic is also used in agricultural products, as a hardening agent for bronze and other alloys, in glassmaking and, in a highly purified form, in the manufacture of computer chips.
Deposits of arsenic were mined extensively in the United States from the mid- to late-1800s. New Hampshire, the primary domestic source for many decades, was known at the time as “the Arsenic State.” Since 1986, no arsenic producers have operated in the United States. Raw materials needed to produce arsenic-containing products are now imported.
How does Arsenic get into Food and Water?

Arsenic enters the food web when it is taken up from soil by plants that are eaten by animals, or when it is taken up from water by algae or plankton that are eaten by fish. Arsenic does not appreciably accumulate in the body over time (bioaccumulate) and it does not increase in concentration as it moves up the food chain (biomagnify). It is readily excreted by animals.
Fruits and vegetables generally contain extremely small traces of arsenic. Slightly higher – but still tiny – amounts may be found in animals, particularly aquatic species that filter water, such as shellfish. In general, foods are not a major source of arsenic toxicity for humans. For example, the arsenic found at high concentrations in fish tissues, called arsenobetaine or fish arsenic, is a non-toxic form that is easily eliminated by the body.
Arsenic in drinking water is of far greater concern. Underground water flowing over arsenic-rich rock may become contaminated with high concentrations of a toxic form of arsenic, which can make its way into private wells and public water supplies. In certain parts of the world, including areas of Taiwan, South America, India and Pakistan, drinking water may contain arsenic concentrations as high as one part per million. More recently it has become apparent that geological deposits are also linked to elevated levels of arsenic in drinking water in the United States, including areas in New England and in the Southwest. Arsenic levels in U.S. drinking water are lower than those found in the Southern Hemisphere of the world but are still high enough to raise health concerns.
Though human activities were once believed to be the major source of arsenic in food and water, natural geological sources of arsenic now appear to be a far more significant source.
Do we Need Arsenic for Health?
Studies in animal species provide strong evidence that arsenic is an essential trace element – at least for birds and mammals. When researchers completely eliminated arsenic from the diets of animals in experiments, the animals became ill; some developed reproductive problems. The offspring of these arsenic-deprived adults were born with developmental problems. Putting a small amount of arsenic back into the animals’ diets completely reversed these effects.
Dietary requirements for arsenic in humans are still controversial. There are trace amounts of arsenic in almost all food and water, air and soil, so it is difficult to find humans who are isolated from all sources of arsenic. There are no known human health effects of arsenic deficiency, if such exist, and the effects observed in arsenic-deficient animals would be hard to detect and characterize in humans. Most investigators believe that it is likely that we receive all the arsenic we need from a normal diet, and there is currently no recommendation for a daily dietary intake for humans.
Nutritionists and toxicologists find themselves on opposite sides of an interesting question when they consider the human health effects of elements such as arsenic. In many cases an element can be toxic at one dose and healthful, even essential for health, at another. If it were somehow possible to eliminate from the environment all traces of elements known to have toxic effects, would this have a negative effect on human health? Because arsenic is ubiquitous in the environment, this question is likely to remain moot.
How does Arsenic Harm Living Things?
Arsenic’s toxic effects largely depend on its chemicaland physical form and how one is exposed. A large single dose that produces an immediate effect is called an acute exposure; a smaller amount over a long period of time that produces a gradual or delayed effect is called a chronic exposure.
At acute exposures, such as in accidental or intentional poisonings, arsenic can displace elements involved in the fundamental chemical processes of cells. For example, arsenic has an affinity for binding to sulfur. Certain enzymes involved in metabolism use the sulfur atom of a cysteine amino acid to carry out their function. If arsenic binds to the sulfur at these sites, the enzymes can begin to behave in abnormal ways or lose their ability to function. Arsenic, in the form of arsenate, can also resemble phosphate, which is used by cells for energy and signaling. By displacing phosphate in enzymes or signaling proteins, arsenic can block energy production and normal cell signaling.
At lower chronic exposures, such as in most environmental or occupational exposures, arsenic appears to indirectly modify the way cells communicate. Recent studies at Dartmouth suggest that arsenic may act as an endocrine disrupter by binding to hormone receptors, interfering with normal cell signaling of hormones through those receptors. Disruption of these endocrine receptors by arsenic in this way may contribute to the development of diabetes, cancer and vascular disease.
Other Dartmouth researchers have found that arsenic may interfere with molecular signals that prompt the cells lining heart and blood vessels to grow. The subsequent build-up of these cells can narrow the passage inside blood vessels, restricting the flow of blood. This may be one of the mechanisms that enable arsenic to contribute to cardiovascular disease and other blood vessel diseases.
Dartmouth researchers are also trying to understand other ways in which arsenic increases the risk of certain kinds of cancer. Unlike many other known chemical carcinogens, arsenic does not cause damage to DNA or cause mutations in genes. Instead, it appears to indirectly modify the way cells behave in ways that increase their probability of becoming cancer cells, perhaps in combination with other carcinogens such as cigarette smoke or other environmental contaminants.
What makes some Forms of Arsenic more Harmful to Humans?
The effect arsenic has on living things is strongly governed by its form or species. Although metals are simple elements, metal atoms can combine into different forms that vary in chemical and biological properties. Some forms of arsenic are highly toxic; others are essentially non-toxic. The reasons are rooted in basic chemistry.
Atoms are made up of a nucleus – a mixture of positively charged particles called protons and neutral particles called neutrons — around which negatively charged particles called electrons orbit. The positive, negative or neutral charge on an atom, called its “ionic state,” is governed by how many electrons it has circling around it balancing the positive charges of its protons. Atoms can gain or lose electrons to change their ionic charge, and the sharing of electrons is primarily how atoms bond together to form molecules.
The most common and stable forms of arsenic in nature are arsenite, also called or arsenic (+3), and arsenate, or arsenic (+5). Arsenic (+3) is arsenic with three fewer electrons than protons, giving it a plus three positive charge; arsenic (+5) is arsenic with five fewer electrons than protons, giving it a plus five positive charge. These two forms can be readily converted back and forth both in nature and inside our bodies depending on the local chemical environment – such as changes in acidity (pH), the presence of oxygen or iron, and what other molecules are present. Arsenite is believed to be slightly more toxic than arsenate, but since they are so easily inter-converted, both forms are considered a health risk.
Once arsenic (+3) or arsenic (+5) atoms combine with other elements to form molecules, the molecules acquire chemical and biological properties of their own. When arsenic binds to elements such as sulfur, oxygen, and chlorine it forms molecules known as inorganic compounds; when arsenic binds to molecules containing carbon it forms organic compounds. Inorganic forms of arsenic are, in general, more toxic to humans since they are less stable and may allow arsenic to interact with important cellular molecules.
Both the inorganic and organic forms of arsenic are readily eliminated from the body through the urine. When we are exposed to inorganic arsenic, the body routinely changes, or metabolizes, it into one or more organic forms by successively adding carbon atoms to it. Scientists once believed that this process – known as methylation – was a natural arsenic detoxification process for both humans and other animals.
But new findings have challenged that idea. Animal species that do not methylate arsenic are not only able to excrete inorganic arsenic efficiently but appear to be no more sensitive to its toxic effects than animals that methylate. More recently, scientists have found that a simple methylated form of arsenic called mono-methylarsenic (III) can cause cancer in animals. On the other hand, fish and other animals contain a highly methylated form of arsenic called arsenobetaine or “fish arsenic” which is essentially non-toxic and is readily eliminated by our bodies. So although fish may have high amounts of arsenic in them, it is primarily in a form that is not a health risk to humans.
There is evidence that humans and other animals can build up tolerance to the toxic effects of arsenic. A society of “arsenic eaters” who deliberately consumed arsenic-laden soils in their religious practices developed a high tolerance for arsenic. Rasputin was reported to regularly ingest arsenic to build tolerance and to protect himself from poisoning.
What Amount of Arsenic is Toxic to Humans?

Like any other poison, whether an exposure to arsenic is harmful largely depends on its chemical and physical form and how one is exposed. Toxicologists use the terms dose, duration and route of exposure, meaning the amount of a substance taken in, the period of time the exposure lasts, and the way the substance enters the body. One way of being exposed to arsenic is by breathing it in as a dust. This primarily occurred in workplace settings where arsenic or products containing arsenic were used, and before new knowledge led to the development of modern worker safety measures. There is normally little or no uptake of arsenic through the skin at environmental levels, though it was of concern in previous workplace exposures (such as long-term use of arsenic-containing pesticides) or through use of arsenic-containing medications applied directly to the skin. The route of exposure of most concern today is ingesting arsenic, particularly through drinking water contaminated by inorganic arsenic.
The concentrations of arsenic found in the heavily contaminated drinking water of Bangladesh are between 170 and 1500 micrograms per liter (A microgram is a millionth of a gram). By contrast, a person would have to ingest more than 70,000 micrograms of arsenic all at once to be fatally poisoned by a single dose. Nevertheless, exposure over a long period of time to concentrations of arsenic such as those found in Bangladesh is associated with a wide range of illnesses.
Much of the world’s current safe drinking water standards for arsenic are based on risk estimates using data on people exposed to very high levels of arsenic through their occupations or through drinking water in areas such as Bangladesh, Taiwan and parts of South America. Few studies have examined the effects of lower doses on people over long periods of time.
Dartmouth researchers are conducting epidemiological studies to determine the health effects of drinking water containing arsenic at the elevated levels found in certain regions of the United States. These levels -typically between 50 and 200 micrograms per liter – are much lower than those of Bangladesh but are still considered high enough to be of concern.
Can Arsenic Cause Cancer?
Like many chemicals, arsenic’s effects on cancer at first appear paradoxical. On the one hand, arsenic is one of a handful of chemicals that is well established as a human carcinogen based on direct evidence in human populations. In fact, this was evident in humans long before there was evidence for arsenic’s cancer-causing effects in laboratory animals. On the other hand, arsenic has been shown to be effective as a cancer chemotherapy drug and can be used to induce complete cures in certain forms of cancer.
Surprisingly, it has been difficult to demonstrate that arsenic can increase the incidence of cancer in animals despite the strong human epidemiological data. This is also true of several other carcinogenic metals including chromium, cadmium and nickel. The reasons are unclear, but one view is that these agents act indirectly, by increasing the risk of cancer from other factors. This would not be evident in experiments in which animals are raised in a relatively pristine laboratory environment and exposed only to the metal in question.
Beginning around the 1970s, the Chinese began to systematically experiment with the use of arsenic to treat certain cancers. Most of these studies were published in the Chinese medical literature, which did not become accessible to the western world until the late 1980s. In particular, the Chinese demonstrated that use of arsenite -inorganic arsenic trioxide – was highly effective in treating certain leukemias. Arsenite was particularly useful for people whose leukemias were resistant to chemotherapy treatment using retinoic acid, a derivative of vitamin A. The results of these arsenic studies were recently confirmed in a small U.S. cancer trial as well. These studies suggest that arsenic may prove to be an effective anti-cancer agent for other malignancies in the coming years.
Arsenic’s paradoxical behavior as both cause and treatment for cancer is an example of an often-repeated maxim attributed to Paracelsus, a physician and alchemist who lived 500 years ago: “the right dose differentiates a poison from a remedy.”
What are the Symptoms of Arsenic Poisoning?
Arsenic has been the poison of choice since antiquity because it is difficult to detect in food and water and because the symptoms of poisoning by arsenic can be mistakenly attributed to many other ailments.
The effects of arsenic poisoning differ depending upon whether the exposure is acute – a large dose in a short period of time – or chronic – lower doses over an extended period of time.
At a very high, single dose arsenic can cause severe shock, general paralysis, delirium and then death within a few hours. At a somewhat lower dose the primary symptoms are nausea, headache, intense gastrointestinal pain, vomiting and diarrhea. This can be followed by extensive gastrointestinal bleeding, loss of blood pressure and a decrease in brain function followed by death. These effects are rare except in cases of intentional poisoning or suicides.
Workers and others who have been exposed to arsenic over long periods of time, principally by breathing it or ingesting it, can exhibit symptoms that include melanosis, a change in pigmentation of the skin similar to freckling; hyperkeratosis, an extensive thickening of the skin, especially the palms of the hands and soles of the feet; damage to heart and blood vessels; a decrease in both red and white blood cell production; and severe inflammation of the liver.
These symptoms are also seen in people who live in regions where drinking water contains between 100 and 1,500 parts per billion of arsenic.
Drinking-water arsenic at these levels is also associated with an increased risk of diabetes mellitis (type 2 or adult-onset diabetes), with damage to heart and blood vessels and, in some areas of the world, a condition called blackfoot disease. This causes the feet or sometimes hands to lose circulation and to turn “black.” There is also a strong association between arsenic in drinking water and an increased risk of lung, skin, bladder and other cancers.
Arsenic is cleared from the body quickly, so the most important remedy for arsenic poisoning is eliminating exposure. The most serious effects of arsenic, such as cancer and diabetes, are believed to require long, continuous exposures perhaps lasting 20 years or more.
In cases of extreme poisoning, chemical compounds called chelating agents can be used as an antidote. Chelating agents such as “British anti-lewisite” (BAL) and other more modern therapies work by binding arsenic tightly in complexes, making it inactive. This can help remove arsenic from a person’s body, averting severe toxicity and death.
How can I tell if I’ve been Exposed?
Medical tests can detect arsenic in the human body, but these tests are not part of a routine physical. They may be ordered when there is reason to suspect a person has received a harmful dose of arsenic.
The body routinely excretes arsenic in urine, so a urine test may show whether a person is taking in harmful amounts of arsenic. But since the body metabolizes and eliminates arsenic quickly, a urine test is not useful in telling if someone has taken in arsenic in the past.
Because of arsenic’s affinity for sulfur, it binds tightly to proteins in the human body that contain sulfur atoms. Hair, fingernails and toenails are made primarily of keratin – a stable protein that contains sulfur – so they provide a good means of detecting arsenic exposure in people. Hair and nails grow slowly over time, leaving a record of arsenic exposure for six months to a year. Toenail arsenic is considered the most accurate measure of exposure information because, unlike hair and fingernails, they are less susceptible to contamination from arsenic in soaps, shampoos, air pollution and other sources in the environment.
Who Monitors Arsenic in Drinking Water?

In the United States, the Environmental Protection Agency (EPA) monitors public drinking water supplies under the Clean Water Act. One way the EPA controls the safety of public water supplies is by setting and enforcing a safety standard, or Maximum Contaminant Level (MCL), for drinking water pollutants. The MCL for arsenic of 50 parts per billion was set in 1942, when far less was known about the effects of arsenic on human health. Most other countries of the western world have a current MCL for arsenic of 10 parts per billion.
In 1996 the Safe Drinking Water Act directed the EPA to propose a new standard based on the current level of scientific knowledge concerning arsenic’s effects on human health. The EPA asked the National Research Council (NRC), an independent committee of scientists from the National Academy of Sciences who evaluate scientific problems to guide policy in the United States, to do a detailed review of the scientific literature on arsenic and to make recommendations regarding a new drinking water standard. In 1999, the NRC issued a report that called for the EPA to immediately lower the MCL for arsenic in public water supplies based on what the Council felt was strong evidence of human health effects close to the current MCL.
In January 2001, after a period of review and comment, the EPA recommended a new standard of 10 parts per billion, which was signed into law by President Clinton. In March 2001, implementation of this new standard was revoked by the new Bush Administration pending further scientific and policy review. The NRC was asked to update its 1999 review, and it issued its revised report in September 2001. This report concluded that there is even more compelling evidence from the most recent studies that drinking water arsenic has measurable human health effects at or evens below the current U.S. MCL. On October 31, 2001, after reviewing the new analysis, EPA once again recommended a standard of 10 part per billion. Once a new standard is put in place, it will be implemented by public water supplies over the next decade.
It is important to know that the EPA does not regulate private well owners or by states, so people who draw their drinking water from private supplies are responsible for monitoring its quality and safety themselves. In many areas of the U.S., a large proportion of the population falls into this category. A recent study by Dartmouth researchers found that approximately 40 percent of the residents of New Hampshire use water from a private well, and approximately one-fifth of those wells contain water with arsenic levels above 3 parts per billion. One in ten wells was found to be above the proposed new standard of 10 parts per billion. In some cases, well water contained arsenic at levels considerably higher than the current standard of 50 parts per billion.
It is important for private well owners to have their water tested for arsenic and other contaminants. Arsenic is now included in New Hampshire’s standard well water test and in many other states in recognition of this issue. If arsenic levels are found to be high, homeowners can decide whether to install a system to remove arsenic or to switch to an alternative drinking water source.
Current evidence suggests that other uses of this water (bathing, washing clothes, etc.) do not pose a significant health risk, though this is under active investigation by several research groups. Homeowners should contact their state’s Department of Environmental Services or equivalent agency to obtain more information about testing and remediation options.
How can I tell if there is Arsenic in my Drinking Water?
Arsenic dissolved in drinking water cannot be detected by sight, smell or taste, so the only way to tell if arsenic is present is to have the water tested by a laboratory.
Public water suppliers are required by federal law to test for arsenic and to take measures to ensure that water does not contain levels of arsenic that exceed federal safety set by the U. S. Environment Protection Agency (EPA). The EPA’s web site on drinking water contains annual drinking water reports from each state.
Federal drinking water regulations do not require private well owners to test or remediate their water however. People who use private wells near concentrated sources of arsenic such as waste sites or in regions of the United States where there are geological sources of arsenic should have their drinking water tested by a certified lab. For a list of certified labs, phone your state environmental services department, or the equivalent state agency.
Can Arsenic be Removed from Drinking Water?
Water treatment devices are currently available and can be installed on a single water faucet (point-of-use system) or on a plumbing system that serves an entire residence (whole-house system). Another option is to use bottled water for drinking and cooking. A third solution is to connect to a public water supply, or to construct a new well, though the possibility of tapping another arsenic-rich source should be evaluated.
Contact your state department of environmental services for advice on finding water treatment equipment and services.