Our research agenda includes taking an ecological approach to problems in human environmental health, especially exposure to arsenic as a non-point source contaminant. We’re also getting back into the ecology of infectious disease for the first time in more than a decade.
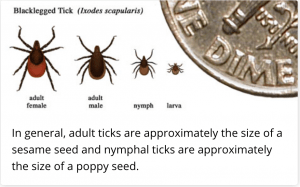
- Lyme Disease: Graduate student Kaitlin McDonald is studying the ecology of the black-legged tick, which carries multiple tick-borne diseases, including the bacterium that causes Lyme disease. Current efforts include field observations to inform our understanding of the factors that determine the factors influencing the distribution and abundance of ticks in northern climates, as well as pilot studies in the laboratory to look more directly at how tick physiology and behavior change with relative humidity. Future studies will likely involve the community ecology of tick vectors, linking back to Kathy’s early work on food webs and trophic cascades. This is our first foray into infectious disease research since studies of the ecology of cholera in the early 2000s.
- Science Communication & Misinformation: Kaitlin, Emily D’Iorio, and I have recently received a grant from Facebook to evaluate the potential to use microinfluencers as digital community health workers to combat misinformation about ticks and tick-borne disease in public Facebook groups. That work will begin in Fall 2020, and will engage with new research partners from the social sciences.
- Arsenic: Kathy is wrapping up a project with Dr. Margaret Karagas and colleagues to assess human exposure to arsenic and other metals. Chronic, low-level exposure to arsenic is associated with skin lesions; skin, lung, and bladder cancer; vascular diseases; low birth weight; increased susceptibility to infection; and reduced IQ. Humans are generally thought to be exposed to the more toxic, inorganic form primarily through drinking water, which is of particular concern in some regions of New Hampshire as well as other parts of the world. In addition, an emerging body of work suggests that elevated concentrations of arsenic in common food items – including rice and rice-based products, fish and seafood, and beer/wine – may pose an additional risk to consumers (see e.g., this update from Consumer Reports). Studying arsenic exposure in food is particularly hard because (1) only some of the arsenic is in the highly toxic inorganic form — and this fraction varies even within types of foods and (2) the toxicity of many organic forms has not yet been established. However, understanding this pathway to exposure is quite important because everyone is exposed to trace amounts of arsenic via food, regardless of the arsenic in their drinking water.
Working as part of the Children’s Center for Environmental Health and Disease Prevention Research at Dartmouth, we are quantifying exposure to arsenic via water and food for members of the New Hampshire Birth Cohort (NHBC), a prospective cohort study that recruits pregnant women who drink water from private wells. To date, our work has shown that rice and products made from rice, such as brown rice syrup, may be quite high in arsenic (Jackson et al. 2012a,b) and may be important sources of exposure for the pregnant moms (Gilbert-Diamond et al. 2011), NHBC infants (Carignan et al. 2015), and in U.S. children more generally (Davis et al. 2012, Lai et al. 2015). Importantly, we are not only assessing exposure as the NHBC children grow from infancy through age 5, but relating those exposures to key health outcomes, including immune function, growth and neurodevelopment.