Just a decade ago, few could have foreseen the current power of brain-machine interfaces (BMIs), devices that intimately link brains with artificial devices like computers and robotic limbs. A new frontier in neuroscience, the BMI field is highly multidisciplinary, spanning biology, mathematics, control and information theory, and material science and engineering (1). The first seed of this technology was planted two centuries ago with the concept that groups of neurons directly control voluntary motor ability. In 1999, when ensembles of cortical neurons first directly controlled a robotic manipulator, BMIs were propelled forward, capturing the interest of both scientists and the public (2).
BMI-based techniques may be the next great leap in fully restoring motor functions in a paralyzed or amputated body. While astounding work has been done to decode the language of the nerves and to translate this language into meaningful motor functions via a computer interface, much development awaits. This paper will begin by presenting a brief overview of paralysis, a devastating medical condition that affects more than five million individuals in the United States alone, following with a discussion of state-of-art BMIs, and finally examining how this developing technology may be used in the future (3).
Medical Need
Resulting from severe damage to the central nervous system, paralysis is one of the most common and debilitating medical conditions, continuing to cast a long shadow of hopelessness on millions of lives in the US. Despite significant research efforts, few therapeutic options are currently available for restoring voluntary motor control of the limbs in paralyzed patients suffering from extensive lesions of their motor system. Worse, “locked in” (severe body paralysis) prevalence is especially high among young adults, primarily due to spinal cord injuries. Caused by auto accidents, violence, and falls, traumatic spinal cord injury accounts for 11,000 new cases annually in the US alone and is one of the leading causes of permanent paralysis (4).
Physiology and Etiology of Paralysis
Paralysis is the loss of voluntary motor function, resulting from disrupted communication between the brain and muscles via the motor pathway, the chain of nerve cells running from the brain through the spinal cord out to the muscles (5). The nerve damage that causes paralysis may be in the brain or spinal cord (the central nervous system) or it may be in the nerves outside the spinal cord (the peripheral nervous system). If the injured nerve has a gap of more than three millimeters, then the nerve cannot heal since nerves have very limited regenerative abilities. The portion of the body which is connected to the brain via the injured nerve loses its function and is deemed impaired.
Spinal cord injury is the second leading cause of paralysis after stroke. Damage to the spinal cord is most often caused by a traumatic event, such as a car crash. Paraplegia (affecting both legs and the trunk) and quadriplegia (affecting all four limbs and the trunk) are the two main types of spinal cord injury with the former mostly caused by acts of violence and mild car accidents and the latter caused by car accidents, falls, and diving (6, 7). Diseases like meningitis, cerebral malaria, diabetic neuropathy and epilepsy can also cause paralysis. Rhythmic control of nerves is lost or altered, causing impairment of the nervous system. Gradual nerve degeneration in the elderly can also lead to paralysis (8).
Insufficient Treatment of Paralysis
There is currently no established treatment to restore the motor functions of a severely paralyzed individual. The primary treatment is a comprehensive rehabilitation program including physical and occupational therapy. This rehabilitation helps make life easier for paralyzed patients, but can do little to restore their motor abilities. Efforts are often made to treat the underlying cause of paralysis when it is due to specific medical conditions. For instance, multiple sclerosis causes dispersed damage to the nervous system and may lead to paralysis, so steroids like prednisone and corticosteroids help alleviate the symptoms of the disease to prevent further damage (9). However, not much can be done to restore the functions of nerves once they are damaged.
For less severe paralysis, a field of reconstructive surgery known as nerve reconstruction is currently available, promising to restore a certain degree of motor function in paralyzed patients (10). However, the outcomes of these surgeries are unspectacular at best. Surgery of the nerves is very unpredictable, riding on the small probability that the nerves will heal themselves and carrying a high degree of risk of further damage to the nerves. Another treatment that is available though not widely used is nerve allograft transplantation, which attempts to repair nerves using healthy donor nerves. However, this requires the patient to be on lifetime immunosuppressant drugs with unpredictable outcomes regarding return of motor abilities (11).
A newer form of treatment currently being investigated is the usage of stem cells to regenerate damaged nerve cells. A recently developed stem cell surgery from Portugal involves removing cells from the injured person’s nasal cavity and transplanting them into the damaged portion of the person’s spinal cord (12). Though promising, these stem cells carry the risk of developing into cancerous growths.
Despite these budding efforts to treat paralysis, the absence of treatment to fully restore mobility in paralyzed patients severely compromises the lives of the millions of paralyzed individuals worldwide. However, the current technology of brain-machine interfaces may serve as a light of hope for the paralyzed.
Historical Highlights that Led to Birth of BMI
In the early 1800s and 1900s, respectively, Thomas Young and Donald Hebb conceptualized independently the idea that electrical activity of large and spatially dispersed populations of neurons, rather than the activity of single cells, is responsible for generating the motor commands required for the production of a voluntary act (14,15). This concept was crucial because to even consider using neuroprosthetic devices to restore motor function in paralyzed patients, motor information must be widely distributed in populations of neurons, thus allowing for random samples of neural populations that would provide sufficient information for movement.
The concept of building a BMI to restore motor function was heavily influenced by the early studies of Eberhard Fetz and colleagues in the 1970s. They were able to develop algorithms to reconstruct movements from the motor cortex neurons that control mobility. These landmark experiments showed that monkeys could learn to increase the firing rate of individual cortical neurons if they were provided with visual or auditory feedback combined with a food reward as part of operant conditioning (16). A decade later in the 1980s, Apostolos Georgopoulos was able to construct a mathematical relationship between the electrical responses of single motor-cortex neurons in rhesus macaque monkeys and the direction that the monkeys moved their arms (17).
The year 1999 marked the rise of brain-machine interfaces with the first experimental demonstration that groups of cortical neurons could directly control a robotic manipulator (18). By 2000, scientists successfully built a BMI that reproduced monkey movements in real time while the monkey operated a joystick or reached for food (19). These historical advances have paved the way to the now fast growing field of BMIs.
State-of-the-Art BMI
The fundamental model of a BMI entails extracting from the scalp or the cortical surface electrophysiological brain signals, which are then processed to measure specific features that reflect the user’s intent, such as amplitudes of evoked potentials or EEG rhythms. These features are then translated into commands to operate a device, such as a word-processing program or robotic limb (20).
Non-Invasive BMIs
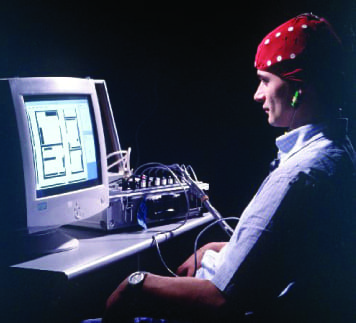
There are two main types of BMIs, categorized by whether they use invasive or non-invasive means of electrophysiological recording. Non-invasive BMIs, or indirect BMIs, use scalp recording electroencephalogram (EEG) electrodes to record electrical signals. The goal is to decode a person’s voluntary intentions and decisions through measurements of the combined electrical activity of massive neuronal populations. Computers act as the decoding instrument, making sense out of various brain signals that act as command sources. Currently, the command output is displayed on a computer screen, which represents the machine component of the BMI and translates intent into action. This system has been successfully used by paralyzed humans to move a cursor on a computer screen (21). Thus, non-invasive BMI is especially useful in helping paralyzed patients develop ways of communication with the external world.
Despite the advantage of not exposing the patient to the risks inherent with brain surgery, EEG-based methods provide communication channels of limited capacity with a transfer rate of 5-25 bits per second, a rate insufficient to control movements of an arm or leg prosthesis with multiple degrees of freedom (22). Further, the resolution of EEGs is limited due to overlapping electrical signals generated by different cortical areas. When passing through bone and skin, resolution is additionally lowered due to the low-pass filtering of the EEG signals. EEGs are also susceptible to other electrical contaminations, including electromyographic, electrooculographic, and mechanical artifacts.
Despite these limitations, EEG techniques are able to detect modulations of brain activity associated with visual stimuli and voluntary intentions, leading to development of several types of EEG-based systems, primarily differing in the cortical areas recorded, EEG signal characteristics, and sensory modality providing feedback to the patients. For instance, one class of EEG-based BMIs makes use of visual evoked potentials (VEPs), which appear when a patient looks at particular items on a computer screen, unveiling the patient’s choice via differing parietal cortex responses to the preferred versus non-preferred stimuli (23).
EEG-based BMIs serve as promising solutions for patients suffering from various degrees of body paralysis. In the case of amyotrophic lateral sclerosis, a motor neuron disease caused by degeneration of motor neurons, these BMIs enable patients to control computer cursors with which to communicate to the external world. One of the first successful applications of this approach was the use of cortical potentials to control a computer-aided spelling system (24). The P300 spelling BMI system flashes letters in rapid succession and the letter that the user wants to select produces a P300 potential, which measures brain response that is directly the result of a thought or perception. By detecting this P300 potential, the BMI system can determine the user’s choice. Another study detailed a tetraplegic patient who was able to produce beta waves in his sensorimotor cortex, activate a functional electrical stimulation device and thereby learn to grasp objects using his paralyzed hand (25). Currently, Toyota is developing a BMI to allow the control of wheelchairs using the mind alone, with 95 percent accuracy (26). Next big question: When will cars come without pedals and steering wheel?
In conclusion, EEG-based BMIs are capable of rendering basic communication and motor control for severely and partially paralyzed patients. Though the motor recovery is limited, these BMIs clearly improve the quality of life of patients, such as the BMI for spelling. However, restoration of movement with multiple degrees of freedom requires recording of high resolution signals from the brain, which is only possible via invasive techniques.
Invasive BMIs
ECoG-based BMI
In order to improve the resolution of brain potentials measured by EEG-based BMIs, slightly more invasive methods like electrocorticograms (ECoGs) are introduced, which record by subdural electrodes. ECoGs sample neuronal activity from smaller cortical areas than conventional EEGs and they measure higher-frequency gamma rhythms (greater than 30 Hz), thereby allowing for better accuracy than conventional EEGs (27). Their clinical use will depend on significant evidence that they are both safe and stable over many years.
Intracortical BMI
Invasive BMIs, or direct BMIs, are intracortical recording devices which record directly from ensembles of single brain cells. They are designed to capture the action potentials of many individual neurons, which are delivered to a computer that processes the signals and converts the commands to movement of the prosthesis or paralyzed limb. This methodology provides neural signals of high quality, but it carries the risks associated with an invasive surgical procedure.
This approach goes back to the aforementioned Fetz and colleagues, who in the late 20th century allowed monkeys to control the activity of their cortical neurons voluntarily, aided by biofeedback. A few years later, Edward Schmidt raised the possibility of extracting voluntary motor commands from cortical neural activity and using these commands to control a prosthetic device to restore motor functions in severely paralyzed patients (28).
Schmidt’s idea accumulated dust and only resurfaced two decades later as technological breakthroughs were able to match his seemingly wild proposition. The primary challenge was gaining access to the action potentials of individual neurons, since microelectrode tips require close proximity to the signal source. Further, electrodes must remain stable for long periods in order to obtain a successful signal and must be biocompatible for patient safety. If higher-order commands and high signal fidelity are desired, the challenge of recording from many neurons simultaneously arises. Microwires have been used for many years for chronic cortical recordings and more advanced multiple electrode array systems are also being designed. One competent design proposed by Joseph Rosen and Gregory Kavacs involves a microelectrode array made of silicon with a layer of iridium that is chemically inert (ideal for biocompatibility). It can endure high current densities (ideal for electrode stimulation) and is perforated with holes so that regenerated axons from nerve cells can loop through the holes and hence become fixed spatially (29).
Currently, humans have been involved in EEG studies and short-term ECoG studies, but have been mostly absent from intracortical BMI experiments which deal mainly with monkeys. Research indicates that EEG-based methods can certainly support simple applications while invasive methods appear able to support complex applications, though before these invasive methods are fully adopted, potential risks and long-term stability must be addressed.
Experimental Technologies
BrainGate: Direct Cortical Control of Devices
The BrainGate neural interface device is one of the first invasive BMI to be tested in humans and is currently in a pilot study involving five quadriplegics. A microelectrode array is implanted on the surface of the brain in the motor cortex area, which controls movement. In the study, a cable connects the sensor to an external signal processor with computers that decode brain activity into useful output commands. The goal is to create a safe design for humans capable of clinical use.
Studies involving monkeys have already established that neural activity can be decoded into command signals that can immediately generate voluntary movements (30). By tapping directly into the cerebral cortex, BrainGate allows for sharper signals and may allow human patients with severe motor impairments to not only control a computer cursor but also eventually control movement of the paralyzed body. The principle behind BrainGate is that with intact brain function, brain signals are generated even though they are not sent to the extremities like the arms, hands, and legs. By taking advantage of the fact that many patients with motor impairment do indeed have an intact brain to produce movement commands, BrainGate creates an output signal directly from the brain bypassing the damaged nerve routes (31).
Input BMIs-Sensory Feeling
Normal human interaction with the external world entails not only converting motor intent to a useful command output signal, but also the ability of sensing or feeling stimuli from the external environment. Hence, an ideal communication interface for paralyzed patients would be the ability to restore sensory pathways that could deliver signals to the cortex, signals that are indistinguishable from a natural stimulus. Through local electrical microstimulation within the cortex, a recent finding revealed the potential of inputting meaningful sensory information to the cortex. Ranuifo Romo and colleagues found that microstimulation of the sensory cortex can mimic perception through skin vibration (32). This finding suggests that humans can regain percepts even when they cannot “touch.”
Ethical Dilemna
One cannot deny the bright future ahead, yet new technology always comes with ethical implications. As brain-machine interfaces become widely used, society must consider many questions regarding science, medicine, and morality.
The first issue is the concept of personal responsibility. When humans contain more and more machine parts rather than flesh, who is responsible for the mistakes? Who is responsible for acts deemed involuntary due to BMI errors-the person with the BMI or the company that made the BMI? In answer to these questions, it is necessary to probe into our long history of ethical dilemmas. It will be very difficult to topple our strong foundation of free will. For instance, even when we began decoding and understanding genetics, people asked whether criminals should take responsibility for their faulty genes and that ended with a firm yes. This new area of neuroscience may be no different. With regards to who takes responsibility for BMI errors, perhaps we have to answer both BMI receiver and BMI maker.
For instance, in the case of pharmaceutical companies, they have the responsibility to rigorously test drugs in order to ensure safety and the patients who are receiving BMIs are responsible for following prescription instructions precisely.
But what if BMIs change the brain? Once we start changing the brain, personalities may change and personalities help define who we are. Take for example Phineas Gage, a man who was very kind hearted before an iron rod pierced his head, making him nasty, mean, and no longer “him” according to people who knew him. Yet, the issues raised are far from new as we look into pharmaceutical drugs like those that help treat depression. Some of those drugs have a disposition to cause suicide and vastly change moods in people taking them. Further, many people undergoing deep brain stimulation for Parkinson’s disease experience hypomania and personality changes that disrupt friend and family relationships (33). In most medical interventions, side-effects are common. In the case of BMIs, the key is to actively identify potential safety issues and to deal with them as efficiently as possible. The classic approach in all medical interventions is to weight the benefits against the risks and to make the decision from there.
Another lingering question is that if the disabled get BMIs, should normal people get them too? Would not the enhancement increase quality of life? Society has not dealt favorably with pure enhancements, such as the classic example of steroids that bestow almost super-human strength, or drugs to increase attention span and improve test results. No system can withstand abuse, but the key is to prevent abuse of the system. BMIs may provide enhancements that could prove beneficial and we should not delay their progress, but before we transition from helping the disadsantaged to enhancing normal human functions, we should better understand what such enhancement entails for society, medicine, and science as a whole.
Looking Ahead
Mankind has outstripped all other species on the planet not due to size, since we are not overpoweringly large, but due to the tools we are able to make to compensate for what we do not yet have. Brain-machine interfaces are one of the most important emerging tools to give those without motor function the ability to move, and therefore regain their autonomy. Humans have come far and brain-machine interfacing will help humans continue the sprint forward.
References
1. A. Rudolph, Brain Machine Interface. (2001). Available at http://www.jameh.org/pdf/BioMagnetics_Rudolph.pdf (15 December, 2009).
2. J.K. Chapin et al., Nat. Neurosci. 2, 664-670 (1999).
3. J. Akre, More than five million live with paralysis, new research shows. (2009). Available at: http://www.injuryboard.com/national-news/more-than-five-million-live-with-paralysis-new-research-shows.aspx?googleid=261456 (15 December, 2009).
4. A. I. Nobunaga, B. K. Go, R. B. Karunas, Arch. Phys. Med. Rehabil. 80, 1372-1382 (1999).
5. Paralysis. Available at http://www.medterms.com/script/main/art.asp?articlekey=4765 (15 December, 2009).
6. Paralysis. Available at http://biology.slss.ie/resources/hi9.pdf (15 December, 2009).
7. W. G. Bradley et al., Neurology in Clinical Practice. (Butterworth-Heinemann, Boston, MA, 1996).
8. What exactly happens in paralysis. Available at http://www.indiastudychannel.com/sites/355/Forum-1217-What-exactly-happens-Paralysis.aspx (15 December, 2009).
9. Treatment for multiple sclerosis. Available at http://www.wrongdiagnosis.com/m/multiple_sclerosis/treatments.htm (15 December, 2009).
10. M. Meek et al., Microsurgery, 17, 555-6 (1996).
11. S. Mackinnon et al., Plastic & Reconstructive Surgery, 107, 1419-1429 (2001).
12. A. Chakraborty, Paralysis Treatment in Portugal from Nasal Stem Cells. (2005). Available at http://stemcell.taragana.net/archive/paralysis-treatment-in-portugal-from-nasal-stem-cells/ (15 December, 2009).
12. New Breakthrough in paralysis treatment reported. (2003). Available at http://www.innovations-report.de/html/berichte/medizin_gesundheit/bericht-23350.html.
13. T. Young, Phil. Trans. R. Soc. Lond. 92, 12-48. (1802).
14. Hebb, D. O., Organization of Behavior. (John Wiley & Sons, NY, 1949).
15. E. E. Fetz, D. V. Finocchio, Exp. Brain Res. 23, 217-240 (1975).
16. A.P. Georgopoulos et al., Science, 243, 234-236 (1989).
17. Chapin, J.K. et al., Nat. Neurosci. 2, 664-670 (1999).
18. J. Wessberg et al., Nature, 16, 361-365 (2000).
19. J. R. Wolpaw et al., Clin. Neurophysiol, 113, 767-791 (2002).
20. J. R. Wolpaw, Suppl. Clin. Neurophysiol. 57, 607-613 (2004).
21. N. Birbaumer, Clin. Neurophysiol. 117, 479-483 (2006).
22. F. Piccione et al., Clin. Neurophysiol. 117, 531-537 (2006).
23. T. Hinterberger et al., Clin. Neurophysiol. 114, 416-425 (2003).
24. G. Pfurtscheller et al., Neurosci. Lett. 351, 33-36 (2003).
25. Brain Power: Toyota develops thought-controlled wheelchair (2009). Available at http://www.autoblog.com/2009/06/29/brain-power-toyota-develops-thought-controlled-wheelchair/ (18 November, 2009).
26. E. C. Leuthardt et al., J Neural Eng. 1, 63-71 (2004).
27. E. M. Schmidt, Ann. Biomed. Eng. 8, 339-349 (1980).
28. G. Kovacs, C. Storment, J. M. Rosen, 39, 893-902 (1992).
29. Serruya et al., Nature, 416, 141 (2002).
30. S. Arjun, ICBME, 1232-1235 (2008).
31. R. Romo et al., Neuron, 26, 273-8 (2002).
32. G. Pfurtscheller et al., Neurosci. Lett. 351, 33-36 (2003).

Leave a Reply