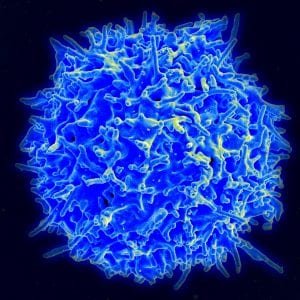
Normal human T cells, which are white blood cells involved in the immune response, are regulated by molecules that bind to surface receptors. Researchers at MIT recently demonstrated that one such signaling molecule, known as IL-17a, can produce autism-like symptoms in mice. (Source: Wikipedia, Credit: NIH, NIAID)
Autism spectrum disorder (ASD) is typically characterized by reduced social interaction, repetitive behavior, and fixations on certain objects, although individuals with autism often express unique sets of symptoms (1). Mice models have been used to show that viral and bacterial infections in the mother during pregnancy, combined with the corresponding immune response, are linked to autism-like behaviors in offspring. Now, research from a team of scientists at the Massachusetts Institute of Technology provides new insight into the molecular mechanisms behind this phenomenon. The researchers provide evidence that the cytokine interleukin-17a (IL-17a) must be present during the immune response in order to produce autism-like symptoms (2).
The signaling molecule IL-17a interacts with TH17, a type of white blood cell involved in immune responses against bacteria and fungi, to produce the immune response (2). A 2010 Danish study showed that mothers who experience viral or bacterial infections during pregnancy tended to have children with autism (3). In addition, previous studies showed that children with autism tended to have higher concentrations of IL-17 in their blood (2). As a result, IL-17a was suspected to play a large role in generating the symptoms of autism (2).
To test their hypothesis, researchers artificially triggered an immune response and inflammation in pregnant mice and observed that both the mice and their offspring exhibited elevated levels of IL-17a (2). Further examination showed that offspring also had underdeveloped cortical structures, although cortical thickness remained within normal parameters, reduced vocalizations, and decreased social interaction, all symptoms typically associated with autism (2). In addition, injections of IL-17a into the brains of fetal mice produced similar symptoms, and treatment with IL-17a blocking agents partially reversed the effects, providing evidence that IL-17a plays a direct role in regulating neuronal development in the fetal brain (2, 3).
However, because this experiment was done in mice models, researchers are cautious to draw conclusions linking the results of this study to humans. Further research into the IL-17a signaling pathway in humans is necessary and could provide a greater understanding of autism spectrum disorder, as well as a potential method of reducing the prevalence of autism in children born to mothers who contracted infections during pregnancy (3).
Works Cited:
- Autism Spectrum Disorder. (n.d.). Retrieved January 31, 2016, from http://www.nimh.nih.gov/health/topics/autism-spectrum-disorders-asd/index.shtml
- Choi, G. B., Yim, Y. S., Wong, H., Kim, S., Kim, H., Kim, S. V., … & Huh, J. R. (2016). The maternal interleukin-17a pathway in mice promotes autismlike phenotypes in offspring. Science, aad0314.
- Massachusetts Institute of Technology. (2016, January 28). How severe maternal inflammation can lead to autism-like behavior: Immune molecules in infected mothers tied to brain and behavior abnormalities in offspring.ScienceDaily. Retrieved January 31, 2016 from www.sciencedaily.com/releases/2016/01/160128152147.htm
Contact brenda.y.miao.19@dartmouth.edu with questions.
Leave a Reply