Nishi Jain 21′

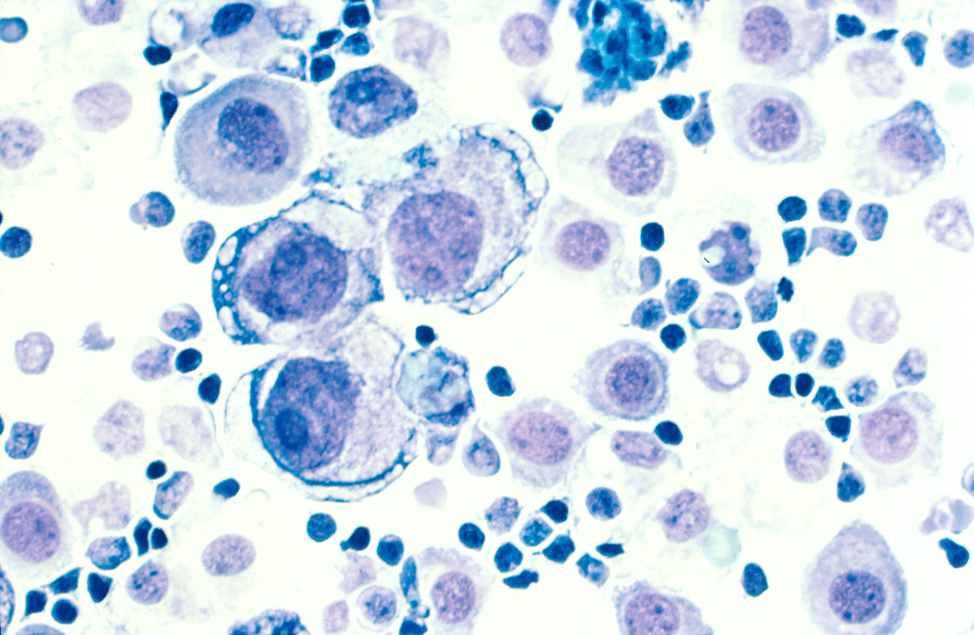
Tissue culture experiments frequently involve the use of cancer cells similar to these.
(Source: Wikimedia Commons)
Although it is one of the most common cancer diagnoses for women in America and across the world, breast cancer has also been one where breakthrough therapies have been highly efficacious and able to see affected women through to a complete or near-complete remission. Such therapies have historically included surgery, chemotherapy, hormonal therapies, biological therapies, and radiation therapies. However, surgeries like lumpectomies and mastectomies can only be performed if the danger of surgery is minimal and the patient agrees the procedure.1 And other radiation therapies are often used as a follow-up, targeting the tumor with high energy external beams that kill the residual tumor cells.2
If patients opt out of surgery, they are often given a number medications, one of which is chemotherapy that is administered orally or via IV. Chemotherapeutic agents shrink tumors by disrupting tumor cell machinery or inflicting DNA damage to cancerous cells. Additionally, hormonal therapies are common, as cancers often require estrogen to continue growth – hormone-sensitive cancers are identified through tumor biopsies, which can reveal the presence of certain estrogen or progesterone receptors (cancers with these receptors are labeled ER+ and PR+ respectively).1
These techniques are all proven localized treatments for tumors that are small and operable, but there are other situations in which conventional therapies do not work. For instance, tumors frequently develop immunity towards the medications and begin to mutate such that hormonal therapy becomes ineffective.1 In the face of such changes, additional therapies must be developed to treat patients with inoperable and mutated tumors.
A group of scientists at the University of California Davis, Central South University, and the National Center for Nanoscience and Technology have been working to develop peptide nanoparticles that assist in the targeting of HER2 in HER2+ breast cancer. HER2 (human epidermal growth factor 2) is a cell surface antigen present on all cells, but is overexpressed in about 20% of breast cancers (these cancers are thus labeled HER2+).2 Currently, combination therapies of multiple drugs are common, but they require patients to have to visit the physician frequently – an enormous investment of time and money.1 This owes to the fact that the drugs of combination therapy often have different administration timelines.
HER2 is part of the EGFR family of receptors and can signal cell proliferation through activation of protein kinase pathways. A necessary precursor to cell signaling activity is either the homodimerization of one HER2 molecule with another or the heterodimerization of HER2 with another member of EGFR family. This dimerization event sends signal cascades through the cell and leads to greater cell growth and tumor development1. The nanoparticle developed by the team of scientists can disrupt the dimerization of HER2 and limited cellular cascades.2
The nanoparticle has two different behaviors. Under the regular aqueous conditions where it is prepared, it self-assembles into and appropriate form that allows it to enter the tumor microenvironment. When it comes into contact with the HER2 on the cancer cell surface, it transforms into a set of nanofibrils (wire-like in shape) that stop the heterodimerization of HER2 with another EGFR receptor in the vicinity.2 This action stops the downstream signaling and eventually leads to apoptosis (death) of the cell.
These nanoparticles are a promising potential monotherapy (one that is taken without supplementary drugs) that may reduce time spent in the hospital. It also affords hope to those who have developed immunity toward existing anti-tumor measures.
References:
[1] Harbeck, N., Penault-Llorca, F., Cortes, J. et al. (2019). Breast cancer. Nat Rev Dis Primers 5, 66. https://doi.org/10.1038/s41572-019-0111-2.
[2] Zhang, L., Jing, D., Jiang, N. et al. (2020). Transformable peptide nanoparticles arrest HER2 signalling and cause cancer cell death in vivo. Nat. Nanotechnol. 15, 145–153. https://doi.org/10.1038/s41565-019-0626
Leave a Reply