Anahita Kodali, Medical Sciences, News, Summer 2020
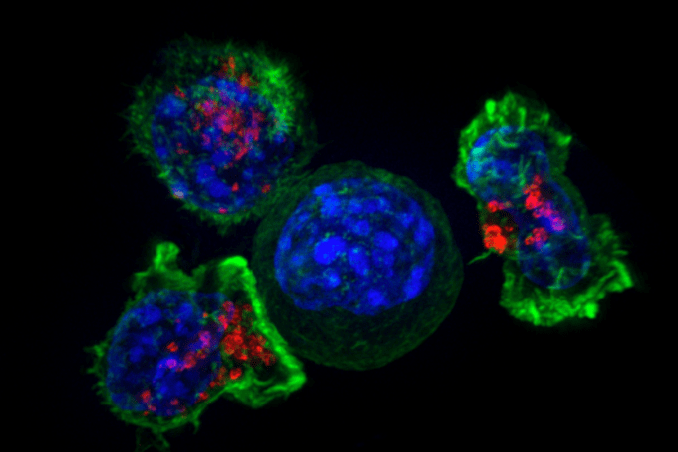
Figure 1: Pictured here are three T cells surrounding and preparing to destroy a cancerous cell. When they come into contact with a foreign cell, T cells attach themselves to the offending cell. They then release chemicals into the foreign cell to kill it.
Image and Information Source: Wikimedia Commons
Tumor immunology, the study of the interactions between the body’s immune system and cancer cells, has become an extremely popular topic among physicians and scientific researchers over the past few years. One of the biggest roles of the immune system is to recognize the differences between the body’s own cells and foreign antigens (foreign proteins that potentially pose a threat to the body and therefore are destroyed by the immune system). Theoretically, the immune system can recognize infinite antigens through genetic recombination, as different genetic combinations can give adaptive immune cells new receptors to recognize new antigens. Because cancer cells have several genetic abnormalities that immune cells may identify and target, it is critical to explore the role that the immune system may hold in halting cancer progression.1
Thus far, immunotherapies have been employed against several types of cancers, including breast cancers, colorectal cancers, lung cancers, prostate cancers, leukemias, and melanomas.2 However, immunotherapies unfortunately are not (yet) the silver bullet to fight cancer because tumor cells have several ways of evading and hiding from immune cells. Many of these strategies are still unknown, but researchers are constantly trying to find ways to both improve the immune system’s responses to tumors and better understand the mechanisms through which tumor cells are able to beat immunotherapy. Following that line of inquiry, researchers from the University of Bonn in Germany were interested in studying the strategies used by melanomas (types of skin cancers) to fight the immune system. The team, led by Dr. Maike Effern, wanted to determine if there was any particularly powerful method for triggering a strong and long-lived immune response. They created a label to tag several different genes active during the melanoma’s developmental phases and used these tags to produce antigens. To complete these steps, they used CRISPR inserted different T-cell epitopes into endogrenous gene products that resided in melanoma cells to get genes of interest; they then designed donor plasmids with fluorescent tags using these genes. They then set off T-cells (a type of immune cell) against the melanoma. These T cells were primed to target the melanoma antigens so the team could study how the melanomas with different tags evaded the cells.3
They found that depending on what gene was tagged, the cancer cells responded very differently. There were two significant findings. First, when genes responsible for melanoma-typical characteristics were tagged, the tumor cells began to suppress these genes over time and would also change their appearance. Therefore, since the alteration of these genes lead to cancer cells ability to change appearance, it was concluded that these genes are responsible for tumors evasion of immune cell capture. Second, and perhaps more important, genes responsible for melanoma-survival are more difficult for the cells to downregulate. Therefore, tagging these cells for immune cell response can potentially lead to more effective immunotherapies as tumors will be unable to hide these genes.3
Both of these findings have important implications for the future of melanoma research and for cancer immunotherapy research in general. One of the authors, Professor Michael Hölzel, commented that “the method [the team] developed also makes it possible to better understand the processes by which cancer cells slip under the radar of the immune system”.4 If researchers can employ their novel approach and determine which cancer genes are responsible for tumor survival, they will be able to develop strategies to tag these genes and engineer better immunotherapies for virtually any cancer.
Bibliography
[1] Raval, R. R., Sharabi, A. B., Walker, A. J., Drake, C. G., & Sharma, P. (2014). Tumor immunology and cancer immunotherapy: summary of the 2013 SITC primer. Journal for ImmunoTherapy of Cancer, 2(1), 14. https://doi.org/10.1186/2051-1426-2-14
[2] Rahma, O. (2020, April 21). What Types of Cancer Can Be Treated With Immunotherapy?: Dana-Farber. What Types of Cancer Can Be Treated With Immunotherapy? https://blog.dana-farber.org/insight/2020/04/what-types-of-cancer-can-be-treated-with-immunotherapy/.
[3] Effern, M., Glodde, N., Braun, M., Liebing, J., Boll, H. N., Yong, M., … Hölzel, M. (2020). Adoptive T Cell Therapy Targeting Different Gene Products Reveals Diverse and Context-Dependent Immune Evasion in Melanoma. Immunity. https://doi.org/10.1016/j.immuni.2020.07.007
[4] University of Bonn. (2020, August 5). How tumor cells evade the immune defense: Study ledby the University of Bonn might help to improve modern therapeutic approaches. ScienceDaily. Retrieved August 7, 2020 from www.sciencedaily.com/releases/2020/08/200805102038.htm

Leave a Reply