Autism and attention-deficit hyperactivity disorder (ADHD) are both neurological disorders that have gained attention in recent years (1, 2). ADHD is much more prevalent in the United States than in Europe, which could be due to either differences in diagnostic procedures, or to genetic and environmental effects (3). The rate of autism diagnosis has increased from 4-5 to 10-12 patients per 10,000 individuals. It is difficult to tell whether this change stems from revisions in diagnostic protocol or from a legitimate increase in the number of affected individuals (1). By looking at what is currently known about the causes of both autism and ADHD, it may be possible to gain insight into the reasons behind these trends. A more complete understanding of the complex etiologies of these disorders may also lead to further improvements in treatment and prevention (1, 4).
Attention-Deficit Hyperactivity Disorder (ADHD)
ADHD is a relatively common neuropsychiatric disorder that affects 3-5% of children, and 5.29% of individuals worldwide (2, 3). There are three accepted subtypes of ADHD: hyperactive-type, which is associated with a high degree of impulsivity, inattentive type, which is characterized by an impaired ability to devote sustained focus on a given task, and the combined type which incorporates symptoms from the each of the two other groups. The majority of patients diagnosed with ADHD fall into the final category. Symptoms usually manifest during childhood, and in approximately half of all cases persist later in life (2).
Research suggests that ADHD may manifest itself somewhat differently in males and females. In children, boys are more likely to exhibit hyperactive-type symptoms, whereas girls generally show more inattentive-type symptoms. Girls with ADHD also tend to suffer more academically than boys with the disorder (5). However, boys are also 2.5 to 9 times more likely to be diagnosed than girls are, perhaps because their symptom profiles tend to be more socially disruptive. Still, it is also possible that boys are simply more susceptible to developing ADHD (2).
Magnetic resonance imaging (MRI) studies of patients with ADHD have demonstrated possible physiological underpinnings of the disorder. Scans of patients with ADHD show a widespread reduction in cerebral volume compared to normal individuals. Furthermore, functional MRI (fMRI) studies have demonstrated reduced activity in the frontal cortex and striatal regions of the brain, which are important for impulse control (2).
Dopamine and ADHD
Recent findings have shown that ADHD may have a genetic component. In studies carried out by Swanson and colleagues, genetic analysis of a series of subjects with ADHD demonstrated evidence of sequence anomalies in the highly variable dopamine D4 receptor (DRD4) gene located on chromosome 11p. In the cell, the DRD4 receptor protein resides in the membrane and is involved in regulation of neuronal signaling in response to its ligand, dopamine (6).
A high degree of sequence variability was discovered within the third cytoplasmic loop of the DRD4 receptor. Sequence analysis of this region of the DRD4 gene showed evidence of variable number tandem repeats (VNTRs) of a 48 base-pair (16 amino acid) sequence that can exist in two to eleven copies within the gene. Patients with seven or more tandem repeats are more likely to exhibit symptoms of ADHD (6).
The DRD4 receptor, which has been localized to the prefrontal cortex, is thought to be important in the regulation of behavioral control. The abnormal allele has also been linked to so-called “novelty seeking” behavioral patterns that are strikingly similar to those associated with ADHD. It is thus hypothesized that an excessive number of repeats could correlate with a reduction in receptor efficacy. This may result in lack of adequate dopamine levels in the prefrontal cortex, possibly inhibiting impulse control (6). ADHD is treated with stimulants such as methylphenidate, amphetamine and pemoline, which function by both stimulating catecholamine release, and inhibiting its reuptake. This leads to an increase in dopamine and noradrenaline levels in the brain, which are believed to be responsible for alleviating the symptoms of ADHD (2, 6).
Still, the abnormal DRD4 receptor hypothesis does not explain why a subject with ADHD symptoms might have normal DRD4 alleles. For such instances, disorder phenotype may be due to neuronal damage during fetal development or early childhood. In the future it will be beneficial to examine possible environmental triggers of ADHD in order to develop both preventative measures and treatments (6).
Autism
Patients with autism exhibit a tendency toward repetitive behavioral patterns, and generally have difficulty interpreting other people’s emotions or mental states. Anxiety problems are also a problem central to the disorder (7). Symptoms of autism generally become apparent by age five and persist into adulthood (1, 8). Familial and monozygotic twin studies have shown that autism is highly heritable, which seems to suggest a genetic rather than environmental origin. Chromosomal abnormalities are commonly associated with autism, with mutations frequently occurring on chromosome 15 (1).
MRI studies have also identified several physiological abnormalities in autistic patients, namely a reduced corpus callosum and an increase in the size and cell density of the amygdala (7, 9). Abnormal brain development has also been noted in autistic patients. The brain grows rapidly from infancy until about 2 to 3 years of age, but this period of rapid growth is followed by slow brain development later in childhood (9). Autism is also associated with chronic inflammation within the brain in areas marked by excessive proliferation of white matter and glial cells (8).
There are several forms of the disorder, with classification depending on the severity of symptoms. Asperger syndrome (AS) is a mild form of autism. Patients with pervasive developmental disorder (PDD) exhibit some of the signs of autism, but do not quite fit the symptom profile for either autism or AS. A 1997 study carried out by the Centers for Disease Control and Prevention (CDC) found that approximately one in every 500 individuals is affected by an autism spectrum disorder (ASD) (8). While it is possible that changes in diagnosis protocol are entirely responsible for the apparent increase in prevalence of the disorder, it remains necessary to rule out the possibility of both genetic and environmental causes (1).
Finding the Cause of Autism
The areas of the brain involved in regulation of social behavior were first determined via animal lesion studies in which social behavior was monitored in response to strategic damage to key areas of the brain. Later studies have utilized fMRI to more directly determine which areas of the brain become activated during social interaction. In a study carried out by Baron-Cohen, participants were given a “social intelligence test” during fMRI scanning. Autistic patients exhibited reduced activation in the orbito-frontal cortex (OFC), superior temporal gyrus (STG), and most predominantly the amygdala. The role of the amygdala in social behavior is further supported by the tendency of patients with pathological lesions in this area of the brain to exhibit a reduction in social function (7).
Single photon emission computed tomography (SPECT) analysis of subjects with autism and other ASDs has shown evidence of suboptimal blood flow to the temporal cortex of the amygdala. Normally, identification of mental or internal emotional states is governed by the left amygdala. This area of the brain is also utilized in the processing of complex facial emotions such as those conveyed by the eyes. Research suggests that patients with autism attempt to compensate for reduced function in the left amydgala by relying on the temporal lobe, an area of the brain normally essential for verbal processing and labeling. Furthermore, the amygdala is responsible for processing extreme emotions such as fear. Abnormal function in this area of the brain could likely result in abnormal fear responses, which is consistent with the anxiety problems experienced by individuals with autism and ASDs (7).
The presence of brain inflammation in patients with autism led to studies examining a possible immunological role in the disease process. In rat studies, viral infection has been shown to result in abnormal neuronal death, inflammation, and hyperplasia of glial cells. Another study demonstrated that 43% of mothers with autistic children had contracted some sort of infection, including influenza-like illnesses during pregnancy, as compared to 26% of mothers in the control group. There has also been fear that certain vaccines might be responsible for an increase in the prevalence of autism, likely stemming from the fact that a preservative added to certain vaccines contains mercury. It is known that brain development is negatively affected by exposure to mercury and other heavy metals. However, rigorous studies have yet to find a definitive link between vaccines and autism (8).
It has also been hypothesized that there may be a link between the measles-mumps-rubella (MMR) and diphtheria-pertussis-tetanus (DTP) vaccines and autism. Serum analysis of patients with autism have demonstrated elevated antibody levels to MMR suggesting that immunization might possibly have triggered an autoimmune response, eventually leading to aberrant central nervous system (CNS) development and autism (8).
Conclusion
Autism and ADHD are both relatively common neurological disorders with etiologies that are both complex and not fully understood (1, 2). As a result, it is difficult to determine whether recent changes in disorder prevalence reflect an increase in affected individuals, or merely a change in diagnostic protocols (1, 3, 4). For ADHD, a more complete understanding of the disorder mechanism may yield more efficient diagnosis and treatment methods.
For autism, looking more closely at possible environmental causes is particularly important given recent worries about a possible link between certain vaccines and onset of the disorder (8). While there is still much to learn regarding the causes of each of these disorders, continued research in these areas may prove to be beneficial to many individuals worldwide.
References
1. J. Liu, Am. J. Hum. Genet. 69, 327-340 (2001).
2. S. Durston, Ment. Retard. Dev. D. R. 9, 184-195 (2003).
3. G. Polanczyk, Am. J. Psychiatry 164, 942-948 (2007).
4. J.M. Swanson, Neurosci. Biobehav. R. 24, 21-25 (2000).
5. M. Gaub, J. Am. Acad. Child Adolesc. Psychiatry 36, 1036-1045 (1997).
6. J. Swanson, Mol. Psychiatr. 3, 38-39 (1998).
7. S. Baron-Cohen, Eur. J. Neurosci. 11, 1891-1898 (1999).
8. H.H Cohly, A. Panja, Int. Rev. Neurobiol. 71,317-341 (2005).
9. P. Brambilla, Brain Res. Bull. 61, 557-569 (2003).
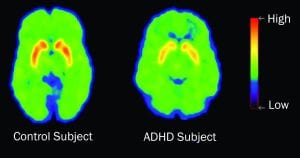
I have noticed that the control subject shows a decreased level of dopamine in the lower mid section of the PET scan. The ADHD has a green, high dopamine transporter in contrast to the blue of the control subject. What area of the brain is this? It seems to me that the ADHD brain is working better than the control subject in this area. Thanks.