Anahita Kodali, Medical Sciences, News, 4/13/2020
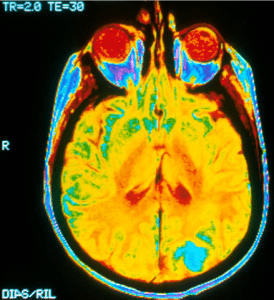
Figure 1: There are several ways that doctors traditionally attempt to visualize brain tumors. This is a magnetic-resonance imaging (MRI) scan of an occipital lobe; the tumor is the bright blue patch found on the bottom right image. These kinds of images are invaluable to doctors, as without them, it would be impossible to find and treat brain tumors.
Image Source: Wikimedia Commons
Brain tumors are notoriously complex and difficult to treat. Annually, over 20,000 adults in the US are diagnosed with some form of brain tumor or cancer1. The average five-year survival rate for adults with brain cancer is about 36%1; in comparison, the five-year survival rate for adults with breast cancer (the most common cancer in the US), is about 86%2. There are several reasons that brain tumors are so difficult to treat when compared to other cancers. For one, since these tumors are in the brain, it is difficult for even very experienced neurosurgeons to surgically remove the tumors due to fear of damaging vital portions of the brain or leaving behind cancerous cells that could grow back. Secondly, the blood-brain barrier, which necessarily protects the brain from large compounds that are normally found in blood, also prevents the vast majority of medicinal drugs from getting into the brain tissue. Additionally, the unique composition of the brain provides a microenvironment for tumors that is very different than more common tumors, so many treatments that are used for other cancers do not work for brain. Finally, because brain tumors are relatively rare, there is less research available to use as a guide for potential treatments3.Thus, it is crucial to develop new research tools and techniques to study the brain and its tumors.
Recently, Kevin Webb led a team of researchers at Purdue University to create a tool that uses optical imaging to map the brain; it can therefore be used to better map out tumors4. After surgeons gives a patient fluorescent agents, the technology uses contrasts in light and fluorescence from the agents to find tumors and blood vessels. This gives the surgeons a good visual of the tumor’s location, which is useful as they develop a course of treatment. With better visualization, neurosurgeons can more accurately remove tumors. Additionally, researchers studying tumor response to treatments are now able to watch the progress of tumor shrinkage easily. This technology is better than current established fluorescent imaging methods, which often have a lot of light scatter that obscures the image5.
Webb’s imaging technology is not limited in its applications in tumor imaging. In general, researchers and surgeons can use it to better understand the brain’s neurological functions. For example, the tool can be used to study neuron activation, which could lead to breakthroughs for other diseases such as Parkinson’s disease4. Ultimately, this novel optical imaging technology will further research in many areas of neurological diseases and contribute to creating better treatments for brain tumors.
Bibliography
[1] Brain Tumor – Statistics. (2020, February 12). Cancer.net. Retrieved from https://www.cancer.net/cancer-types/brain-tumor/statistics
[2] Breast Cancer – Statistics. (2020, February 18). Cancer.net. Retrieved from https://www.cancer.net/cancer-types/breast-cancer/statistics
[3] Aldape, K., Brindle, K.M., Chesler, L. et al. Challenges to curing primary brain tumours. Nat Rev Clin Oncol 16, 509–520 (2019). https://doi.org/10.1038/s41571-019-0177-5
[4] Purdue University. “Optical imaging technology may help surgeons better treat cancer, brain diseases.” ScienceDaily. ScienceDaily, 9 April 2020. www.sciencedaily.com/releases/2020/04/200409113127.
[5] Brian Z. Bentz, Sakkarapalayam M. Mahalingam, Daniel Ysselstein, Paola C. Montenegro, Jason R. Cannon, Jean-Christophe Rochet, Philip S. Low, Kevin J. Webb. Localization of fluorescent targets in deep tissue with expanded beam illumination for studies of cancer and the brain. IEEE Transactions on Medical Imaging, 2020; 1 DOI: 10.1109/TMI.2020.2972200