Dev Kapadia ’23, CS Engineering, 7/16/20
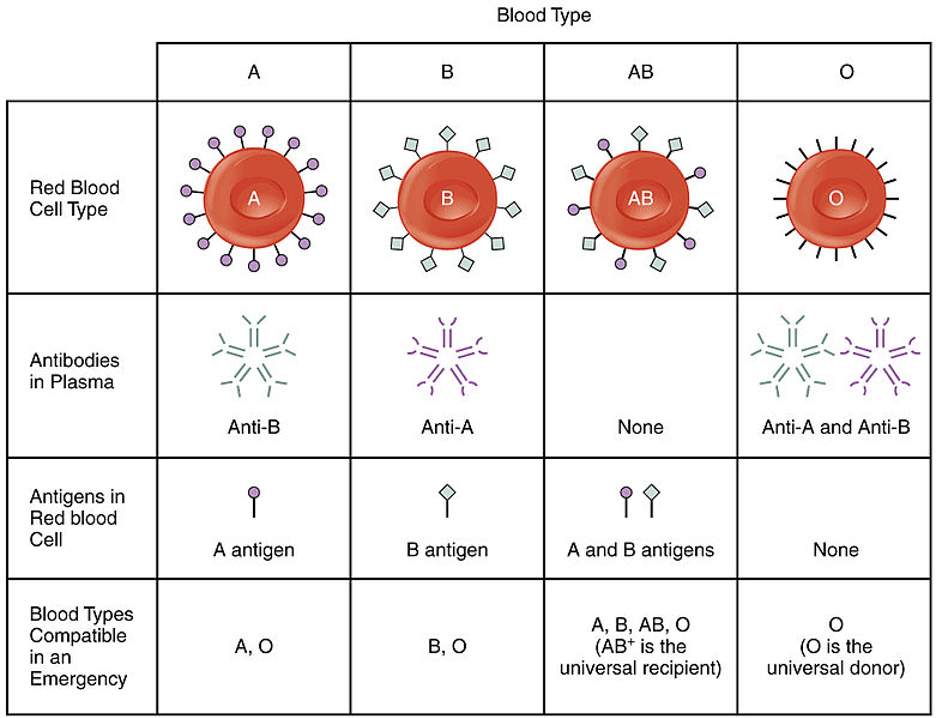
Figure 1: The chart above depicts the breakdown of blood types found in the human body: A, B, AB, and O. As shown, each blood type has compatibility with one or several other blood type groupings. Unfortunately, if an individual receives a blood from a type that it is not compatible with their own, then the blood could clump, and the individual could potentially experience a fatal immune reaction. For this reason, quick and accurate methods or blood type identification could significantly benefit medical treatment, specifically for those who need a rapid blood transfusion.
Source: Wikimedia Commons
Blood transfusions are one of the most critical and regular medical operations. In the United States alone, medical professionals transfuse almost 21 million blood products every year.2 Blood transfusions are the process whereby blood is administered to make up for a lack of blood due to surgery, injury, or some other condition of blood deficiency.3 However, not all blood can be safely administered and used by individuals. In our blood, there are red blood cells, white blood cells, and platelets, but there are also protein molecules called antibodies and antigens.1 Antigens are molecules that, when bound to antibodies produced by the body, elicit an immune response to the foreign molecule that has invaded the body. But, individuals with different blood types express different antigens. The four groups are A, B, O, and AB and whichever one an individual carries depends on whether the individual is a carrier for A antigens, B antigens, neither or both. Further, a blood group can have a positive or negative tag (Rh+ or Rh-) depending on whether the individual carries or does not carry D antigen on their blood cells.4 Unfortunately for recipients of blood transfusions, if the blood group of the donor is not compatible with their own, then the recipient can experience blood clumping (or agglutination). If this occurs, the consequences may be fatal.1
To protect against this possibility, there has been a variety of methods developed to detect the blood group type of individuals. For instance, the centrifugation technique uses a gel matrix and spins a blood sample rapidly for a set amount of time. The blood them separates into its individual components (red blood cells, white blood cells, and platelets). Red blood cells, which agglutinate, are trapped by the gel matrix, while non-agglutinated blood cells are permitted to pass through a column. The blood cells can then be processed and tested to determine blood type. In the microplate technique, various small tubes containing reagents are tested against blood samples and are then centrifuged and incubated to determine for which blood sample types the blood agglutinates, thereby telling of the compatibility of the blood and therefore the typing.1 However, the devices required for these methods are highly-specialized and can take long amounts of time to process (with the fastest methods still taking half an hour); therefore, they are not useful to patients during emergencies.4
To rectify the problem, scientists at Japan’s Tokyo University of Science developed a fully automated chip that can rapidly and accurately determine an individual’s blood type. Within the chip is a miniature laboratory and a corresponding complex process to analyze the blood type of the samples. Once the user inserts a small portion of blood into the chip, the blood is diluted with a saline solution along with air bubbles to facilitate mixing. The diluted blood then gets moved to a homogenizer where the blood is mixed until it is a uniform solution. Lastly, the blood is split and transported to four chambers: one that detects A antigens, one that detects B antigens, one that detects D antigens, and one that is a control (no readings are derived from the control). If there is an antigen-antibody reaction due to the introduction of the respective antibody in each chamber, then the blood will coagulate and the chip will be able to assign that blood group to the individual.4,5
Testing of the device thus far has been promising. Because of the novelty of the device, the initial test only performed on a small sample and served as a “proof-of-concept.” Out of the 10 samples that were tested by the device, all 10 were categorized correctly. Further, the device completed the process in five minutes. The research team hopes that this inexpensive, portable, accurate, efficient chip will lead to more effective and cheaper care for patients in emergency conditions. In fact, there is hope that this technology could be used in aerial medical transport settings, allowing for immediate introduction of care once professionals are within contact of the patient.4 Whatever the application, this technology has significant potential to improve on the medical care currently available.
Bibliography
- Blood Groups, Blood Typing and Blood Transfusions. (n.d.). Retrieved July 16, 2020, from https://educationalgames.nobelprize.org/educational/medicine/landsteiner/readm html
- Blood Needs & Blood Supply. (n.d.). Retrieved July 16, 2020, from https://www.redcrossblood.org/donate-blood/how-to-donate/how-blood donations-help/blood-needs-blood-supply.html
- Mujahid, A., & Dickert, F. L. (2015). Blood Group Typing: From Classical Strategies to the Application of Synthetic Antibodies Generated by Molecular Imprinting. Sensors (Basel, Switzerland), 16(1). https://doi.org/10.3390/s16010051
- Tokyo University of Science. (2020, July 13). A micro-lab on a chip detects blood type within minutes: A novel lab-on-a-chip device reveals the blood type within minutes, holding much potential for use in an emergency. ScienceDaily. Retrieved July 16, 2020 from sciencedaily.com/releases/2020/07/200713120012.htm
- Yamamoto, K., Sakurai, R., & Motosuke, M. (2020). Fully-automatic blood-typing chip exploiting bubbles for quick dilution and detection. Biomicrofluidics, 14(2), https://doi.org/10.1063/5.0006264

Leave a Reply